Abstract
BACKGROUND: Measurable residual disease (MRD) is associated with increased risk of relapse and death in acute myeloid leukemia (AML), even after allogeneic hematopoietic cell transplantation (HCT). Recently, next-generation sequencing (NGS) has emerged as a sensitive and specific method to detect MRD from both bone marrow and peripheral blood. NGS methods are particularly useful for detecting internal tandem duplication mutations of the FMS-like tyrosine kinase 3 gene (FLT3-ITD), which define a subgroup of AML patients who may be at higher risk for relapse and who often undergo consolidative allogeneic HCT. The SORMAIN trial recently reported a highly significant relapse-free survival benefit for the first generation FLT3 inhibitor sorafenib as post-HCT maintenance, particularly among patients with detectable MRD following HCT.
In 2019 our program initiated prospective FLT3-ITD monitoring by NGS using a commercially available assay (Invivoscribe, Inc., San Diego, CA) of the peripheral blood or bone marrow throughout the first three months following HCT for all patients with FLT3-ITD mutated AML undergoing HCT. We encouraged but did not mandate FLT3 inhibitor use, regardless of MRD status. In this study, we describe the clinical impact of sensitive FLT3 MRD testing early after HCT, maintenance FLT3 inhibitor use in a non-clinical trial setting, and the ability of early post-HCT FLT3 inhibitor therapy to modify transplant outcomes.
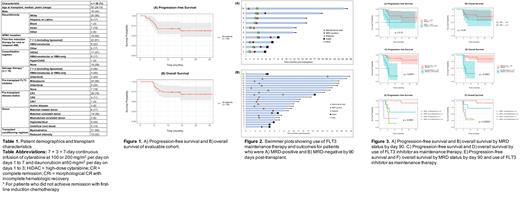
RESULTS: Thirty-six adults with FLT3-ITD mutated AML underwent HCT at Stanford University between April 2019 and August 2020 and were included in this observational study (Table 1). These patients were not enrolled in clinical trials evaluating FLT3 inhibitor therapy after HCT. Twenty-nine (81%) received pre-HCT FLT3 inhibitors, and 78% were in first complete remission (CR1) at HCT. Median follow up after HCT was 14.0 months (range 4.6-25.7). Two patients were excluded from subsequent analyses due to early graft failure and receipt of azacitadine/enasidenib maintenance, respectively. Of the evaluable cohort, 9 (26%) experienced clinical relapse at a median of 4.2 months after HCT (range 1.8-6.1), and 10 (29%) died, 5 from transplant-related mortality and 5 from AML (Figure 1A and B).
Of the 34 patients evaluable for post-HCT MRD analysis, 10 (29%) had detectable MRD within the first three months while 24 (71%) remained MRD-negative (Figure 2A and B). Although there was a trend towards inferior progression-free survival (PFS) for patients with early post-HCT MRD (p = 0.13, Figure 3A), OS was not significantly impacted by MRD (p = 0.35, Figure 3B). Among the four patients with early post-HCT MRD negativity who ultimately relapsed, only one was FLT3-negative at time of relapse.
Twenty-four patients (71%) received FLT3 inhibitor maintenance, initiated a median of 2.8 months after transplant (range 0.7-17.1), and the median duration was 10.6 months (range 1.7-23.7). The most common FLT3 inhibitor used was gilteritinib (n = 15), followed by midostaurin (n = 9), and sorafenib (n = 5). Among the 10 patients (29%) who did not receive post-transplant maintenance, reasons included graft-versus-host disease (GVHD) (n = 4), clinician decision (n = 3), cytopenias (n = 2), and thrombotic microangiopathy (n = 1). The use of maintenance FLT3 inhibitors led to a significantly superior PFS and OS (Figure 3C and D). Interestingly, the use of early FLT3 inhibitors post-HCT augmented PFS and OS in both MRD-negative and MRD-positive patients (Figure 3E and F), and effectively prevented clinical relapse in four patients with post-HCT MRD positivity (Figure 2A).
CONCLUSION: In this cohort study, we evaluated the clinical utility of sensitive post-transplant MRD monitoring and maintenance FLT3 inhibitors on transplant outcomes. We demonstrate that clinical relapse can be prevented even in patients with post-HCT MRD through the incorporation of early FLT3 inhibitors. This finding is in keeping with the results from the SORMAIN trial. We also found that real-time sensitive MRD results allowed clinicians to begin early initiation of FLT3 inhibitor therapy, which positively affected outcomes.
Mannis: AbbVie, Agios, Astellas Pharma, Bristol Myers Squibb, Genentech, MacroGenics, Pfizer, and Stemline: Consultancy; Astex, Forty Seven Inc/Gilead, Glycomimetics, and Jazz Pharmaceuticals: Research Funding. Muffly: Adaptive: Honoraria, Other: fees for non-CME/CE services: , Research Funding; Astellas, Jasper, Adaptive, Baxalta: Research Funding; Pfizer, Amgen, Jazz, Medexus, Pfizer: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal